Nature's Groundbreaking Discovery: Skin as the Body's Largest Immune Organ
Skin: More Than a Protective Barrier
The skin, the body’s largest organ with an area exceeding 1.8 square meters, has traditionally been viewed as a simple "protective shield," primarily preventing pathogen invasion. However, recent research shows that the skin is far from a passive "net." Instead, it serves as a dynamic and complex immune front.
Human skin hosts a vast array of microorganisms, including bacteria, fungi, and viruses. These "commensal microbes"
are not just passive inhabitants; they play an invisible yet critical role in regulating skin health. However, this delicate balance can shift when the skin barrier is damaged or the immune system is disrupted, turning these microbes from “friends” into “foes,” leading to local infections or even systemic diseases.
Rethinking Skin's Immune System
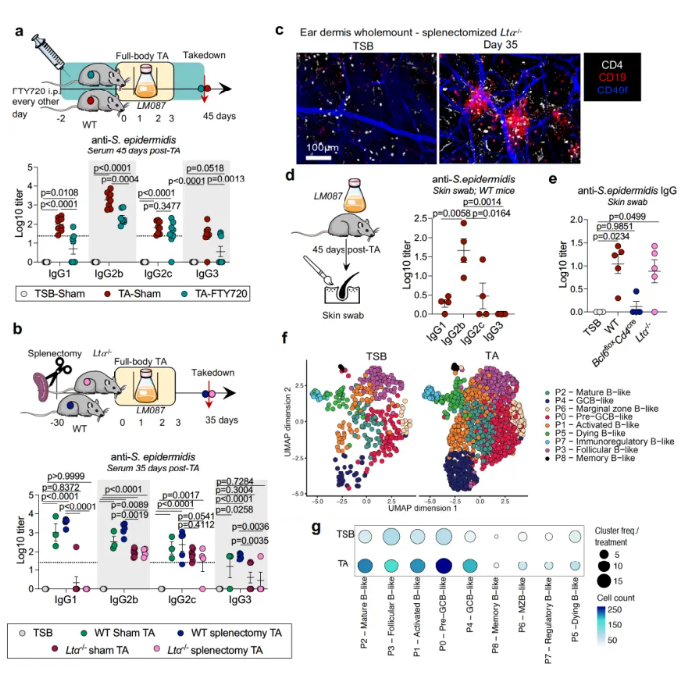
Earlier studies suggested that the skin lacked mature B cells and antibody responses, relying instead on secondary lymphoid organs like lymph nodes for immune regulation. But recent findings reveal that the skin has a degree of "autonomy" in maintaining microbial balance without apparent inflammation.
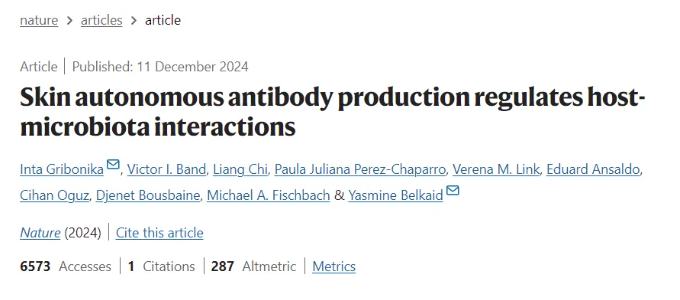
A study published in Nature, titled "Skin Autonomous Antibody Production Regulates Host-Microbiota Interactions," upends traditional views by demonstrating that the skin acts as an "autonomous lymphoid organ." It produces local antibodies to regulate host-microbiota interactions.
Key Findings from the Study
1.Local Antibody Production:
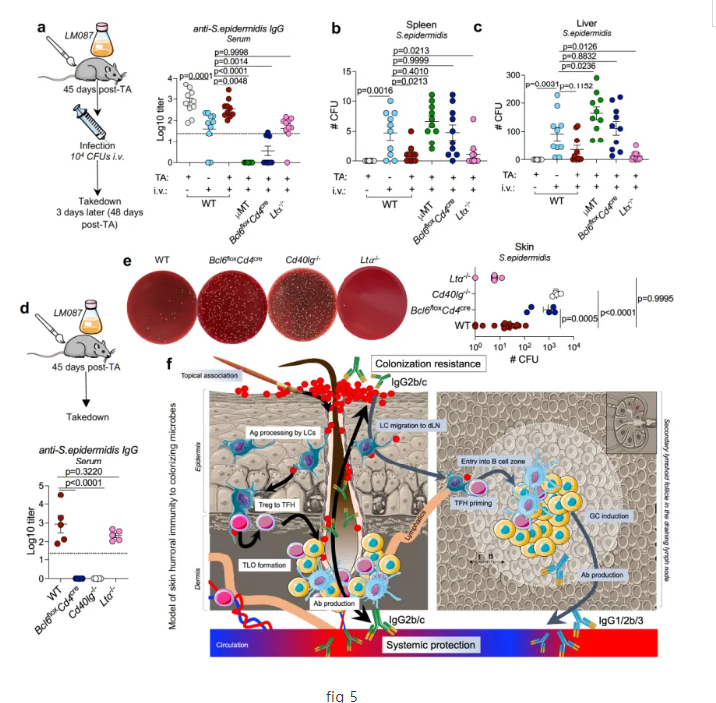
The study highlights that common skin commensals like Staphylococcus epidermidis can induce local production of specific antibodies (IgG2b and IgG2c) in the skin. These antibodies not only limit bacterial growth but also provide systemic protection.2.Long-Term Immune Responses:
Mice colonized with S. epidermidis developed sustained specific antibody responses lasting over 200 days.3.Formation of Tertiary Lymphoid Organs (TLOs):
In response to microbial colonization, the skin forms TLOs that function independently of secondary lymphoid organs, directly promoting antibody responses to microbial antigens.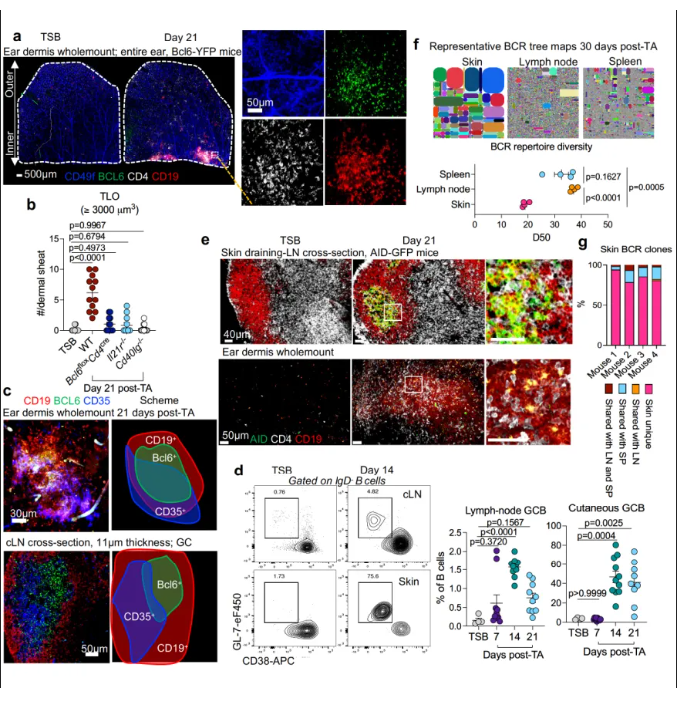
Experimental Design
Hypothesis: Skin commensals induce localized antibody production to control microbial populations and prevent systemic infections.
Methods:
Animal Models: Mice colonized with S. epidermidis.
Flow Cytometry: To analyze immune cell subsets in the skin.
Single-Cell RNA Sequencing: To study B cell functions.
Antibody Detection: Using ELISA to measure specific antibodies in skin swabs.
Histological Analysis: To observe inflammation and lymphoid tissue changes.
Implications of the Study
Host-Microbiota Balance:
The discovery highlights the skin's role in maintaining a balance between microbial symbiosis and immune defense.Innovative Therapies:
Understanding this "immune autonomy" could lead to breakthroughs in treating infectious skin diseases and enhancing vaccine efficacy.
Conclusion
This groundbreaking study redefines the skin as a dynamic immune organ capable of autonomously regulating host-microbiota interactions. By unraveling the skin’s ability to produce local antibodies, this research paves the way for new therapeutic approaches to address skin infections and maintain microbial balance.