Advancements in Psoriasis Treatment: Phototherapy and Medication Combination
1:What is psoriasis?
Psoriasis, commonly known as "psoriasis vulgaris," is a recurrent and chronic skin disease characterized by scaly red patches. Due to its stubbornness and tendency to recur, psoriasis has long been a challenging and troublesome issue for clinical doctors.
2: What are thetreatment methods for psoriasis?
The main treatment methods include UV phototherapy (UV light therapy), traditional Chinese medicine, and Western medicine. Among them, UV phototherapy can be self-administered at home under the guidance of a physician, while other methods require prescriptions and in-person consultations with a doctor.

3: What are the most common types of phototherapy for psoriasis?
There are two types of phototherapy for psoriasis:
(1) Psoralen plus ultraviolet A (PUVA) therapy.
(2) Narrowband ultraviolet B (NB-UVB) therapy.
Narrowband UVB therapy (311nm UVB) is currently recognized as one of the preferred methods for treating psoriasis.
4: What is the principle behind phototherapy using ultraviolet light therapy?
Psoriasis is primarily caused by the activation of certain immune cells in the skin, which produce a large number of inflammatory factors. These factors stimulate the secretion of more inflammatory factors by the cells responsible for forming the outermost layer of the skin (keratinocytes), exacerbating the inflammatory cycle and eventually leading to epidermal proliferation and the formation of psoriatic lesions.
Phototherapy has a dual effect. On one hand, it slows down the proliferation of keratinocytes, reducing the number of cells and thus decreasing the secretion of inflammatory factors. On the other hand, it induces apoptosis (cell death) of immune cells (such as T cells or lymphocytes) that produce inflammatory factors in the skin. By eliminating these cells, the production of inflammation is naturally interrupted.
5: Which types of psoriasis are suitable for phototherapy?
The fewer scales and thinner the skin lesions, the better the effectiveness of phototherapy. The following types of psoriasis are most suitable for phototherapy:
The first category is guttate psoriasis, whether it is initial, generalized, or with larger lesions.
The second category is plaque psoriasis, even if the patient has a large area of skin lesions (greater than 10%, or even greater than 20% or 30%), long-term use of phototherapy is possible.
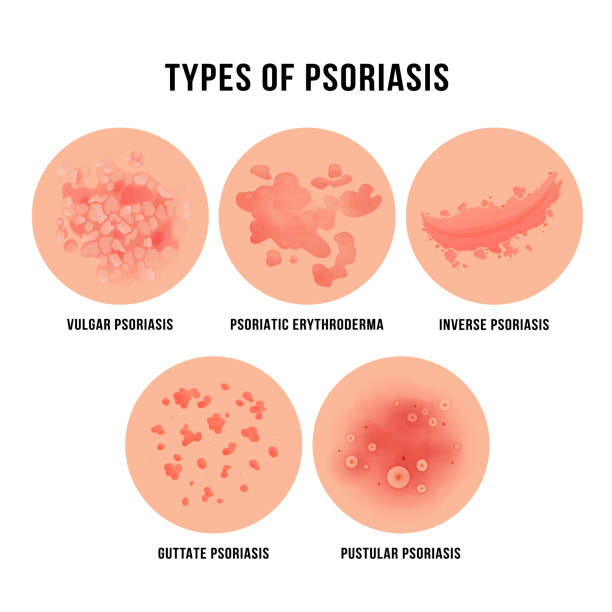
6: Which types of psoriasis are not suitable for phototherapy?
Some types of psoriasis are not suitable for phototherapy. These include progressive erythrodermic psoriasis, pustular psoriasis (the therapy may worsen the condition), and psoriatic arthritis (the joint symptoms do not improve with phototherapy). An experienced physician should make the judgment.
7: Should phototherapy be applied locally or to the whole body?
Phototherapy can be divided into whole-body phototherapy and localized phototherapy. Whole-body phototherapy is suitable for widespread psoriasis lesions, and it requires the use of full-body equipment for irradiation. Localized phototherapy is suitable for single or a few localized and stubborn lesions, using small machines or half-body machines for targeted irradiation. For special areas affected by psoriasis, such as scalp psoriasis, there are now phototherapy combs available. Therefore, depending on the condition, different treatment devices can be selected to achieve the maximum effect through either whole-body or localized phototherapy.
8: How is the dosage of ultraviolet light therapycontrolled?
For an ideal NB-UVB treatment plan, a minimal erythema dose (MED) test should be performed to determine the initial irradiation dosage (mj/cm2): the initial UVB dose is set at 50% of the MED. If the patient's MED exceeds the range determined during MED testing, the initial dose is set at 50% of the highest set dose.
The recommended treatment cycle is three times per week. If there is no erythema on the skin and the interval between the previous and subsequent treatments is within three days, the dosage can be increased as follows: for the first 1-20 treatments, increase each time by 10% of the MED; for the 21st treatment and beyond, the dosage should be decided after consultation with the doctor.
The maximum irradiation dose generally does not exceed 6 MED. After reaching this dose, the dosage is no longer increased.
9: How can the effectiveness of phototherapy be observed?
Thinning and lightening of skin lesions.
Reduction in scales.
Less redness of the skin lesions compared to before.
10: Can I take a shower after phototherapy?
Generally, it is fine to take a shower after about five to six hours of treatment. If you receive treatment at the hospital during the day, you can shower in the evening. If you receive treatment at home in the evening, you can consider taking a shower before the treatment because showering immediately after treatment may weaken the effectiveness of phototherapy.
11: What are the side effects of phototherapy for psoriasis, and how can they be prevented?
Phototherapy for psoriasis is currently considered a relatively safe treatment method. However, no treatment method is 100% free of side effects, and phototherapy is no exception. Just like sun exposure, which is generally safe but can cause sunburn if the sunlight is too intense. However, the risks associated with phototherapy are small, and the damage to the body is relatively low.
The side effects of phototherapy include:
Sunburn: Since phototherapy uses ultraviolet light, sunburn caused by phototherapy is similar to sunburn caused by exposure to sunlight. Mild cases usually subside in about a week. If the sunburn is more severe, the application of topical corticosteroids can accelerate healing. Sunburn can gradually recover, so there is no need to worry too much.
Pigmentation: Skin pigmentation (darkening of the skin) may occur after 1-2 sessions of phototherapy. After about ten sessions, the skin will noticeably darken. However, the skin will return to its normal color a few months after ceasing phototherapy. Apart from these two effects, long-term use of narrowband UVB therapy can cause the skin to become rough and dry, but other long-term side effects are rare.
12: Combining phototherapy with medication
In combination with medication, calcipotriene ointment is a widely recognized and commonly used topical medication with good efficacy for psoriasis. Combining calcipotriene ointment with phototherapy can shorten the time it takes for phototherapy to take effect, reduce the number of treatments, and minimize side effects.
Calcipotriene ointment should be applied topically twice a day, once in the morning and once in the evening. However, it should not be used within two hours before or after phototherapy. Using it before phototherapy can affect the effectiveness of the treatment, and phototherapy can have some negative effects on the medication. After phototherapy, the skin is in a sensitive state, and calcipotriene ointment has a slight irritant effect. Using it during this time may cause some irritation reactions. Once the phototherapy treatment course is completed and the skin lesions are mostly cleared, calcipotriene ointment can continue to be applied to the original lesion sites for a certain period of time to reduce the recurrence rate of skin lesions. Combination therapy must be used under the guidance of a doctor to ensure safety.