Case Report-ALA-PDT Combined with Surgery Successfully Treats Basal Cell Carcinoma(BCC)Within a Sebaceous Nevus:A 6-Month Follow-Up with No Recurrence
2025-03-19 16:23
1. Background
The term "sebaceous nevus" or "Jadassohn sebaceous nevus" was first introduced in 1895 by German dermatologist Josef Jadassohn. It refers to an organoid nevus caused by congenital malformations of the epidermis, dermis, and skin appendages. Meta-analyses indicate that approximately 16% of sebaceous nevus cases may develop benign tumors, while 8% may progress to malignancy. However, the simultaneous occurrence of multiple skin tumors within a single sebaceous nevus is extremely rare.
Genetic mutations may increase the risk of secondary tumors in sebaceous nevus patients, but the exact relationship between primary sebaceous nevi and secondary tumors remains unclear. Due to the potential for malignant transformation, early intervention is crucial to prevent tumor development. However, there is no consensus on whether complete excision should be recommended at the time of diagnosis or on the optimal timing of surgical removal. Some experts advocate for excision before adolescence to prevent growth expansion, while others suggest waiting until the patient can make an informed decision. Full-thickness excision is currently considered the gold standard for sebaceous nevus treatment.
Photodynamic therapy (PDT) has gained popularity as a minimally invasive approach for treating precancerous and malignant skin lesions. This case report details the successful treatment of basal cell carcinoma (BCC) within a sebaceous nevus using ALA-PDT combined with surgical excision.
2. Case Report
Patient Information
Age/Gender: 55-year-old male
Chief Complaint: Raised scalp lesion on the right side, persisting for over 50 years
History: Congenital hairless yellowish plaque on the right scalp, initially the size of a peanut, gradually enlarging and changing in appearance during adolescence. The lesion became mildly itchy, with occasional spontaneous bleeding and ulceration after scratching.
No prior medical consultation despite the lesion’s persistence.
No significant pain, erythema, purulence, or exudation observed.
No history of head trauma, burns, radiation exposure, or skin malignancy.
Clinical Examination
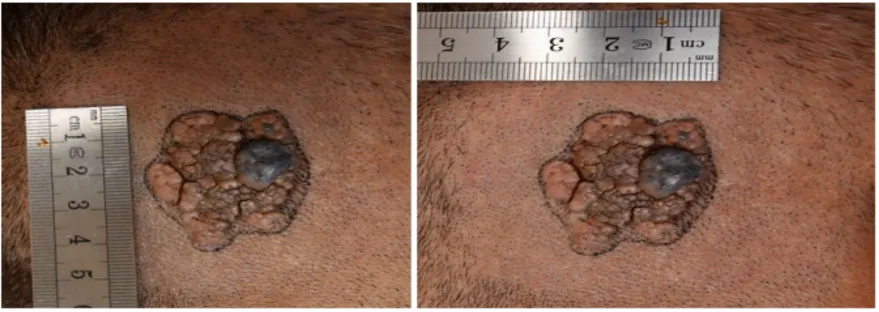
A 3.0 cm × 4.5 cm brown verrucous plaque on the right occipital scalp with no hair growth.
The lesion had a greasy surface with nodular projections.
Adjacent to the plaque, a well-defined dark nodule (0.8 cm × 1.0 cm) was observed.
Imaging & Pathological Findings
MRI: Showed scalp soft tissue swelling, with no intracranial mass.
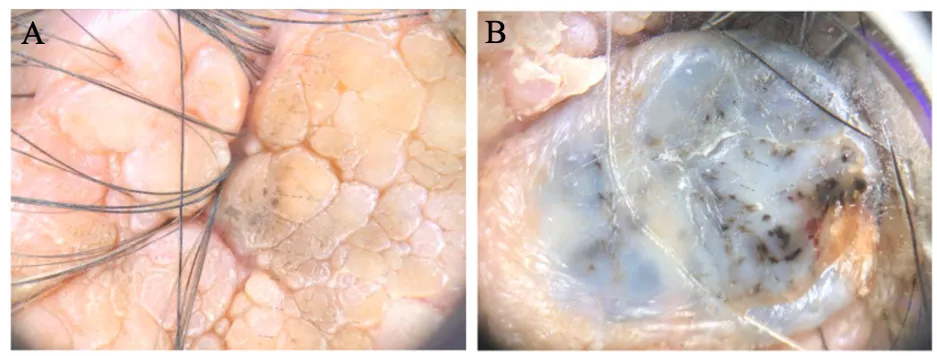
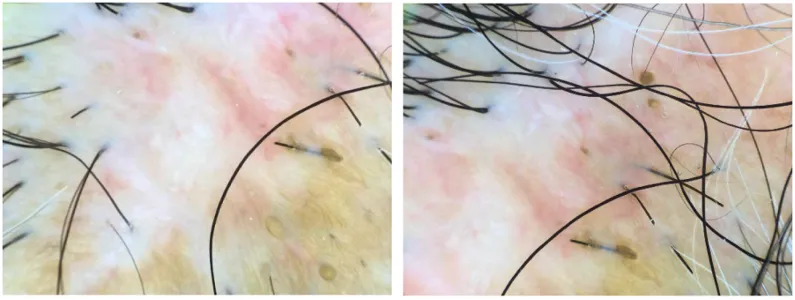
Dermatoscopy:
A brain-like convoluted pattern with hyperkeratotic yellow-red background (Figure 2A).
Multiple round to oval pigmented globules on a light brown background, with scattered brown plaques (Figure 2B).
No prominent vascular structures observed.
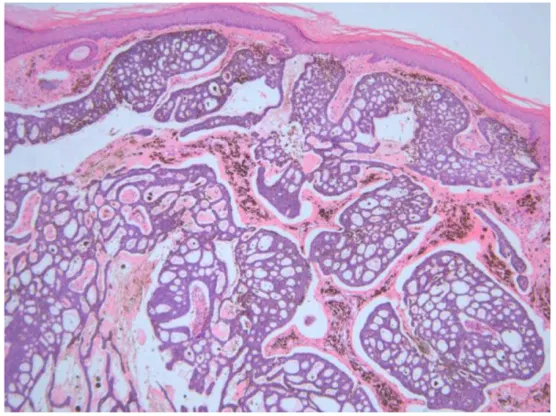
Histopathology:
A 4 mm punch biopsy was performed on both the yellowish plaque and the brown nodule.
The nodule exhibited irregular basophilic nuclei with epidermal invasion.
The presence of palisading basal-like cells and tumor nests with clefting between the tumor cells and stroma confirmed the diagnosis of BCC (Figure 3).
Final Clinical Diagnosis
Sebaceous nevus with secondary basal cell carcinoma (BCC).
Treatment Strategy
The patient underwent surgical excision of the plaque with a 5 mm safety margin.
Following excision, three sessions of ALA-PDT were performed.
ALA-PDT Procedure:
A 20% ALA solution was freshly prepared and applied using a sterile gauze pad.
The lesion was occluded for incubation, followed by red light irradiation (633 nm, 80 mW/cm²) for 20 minutes.
Treatments were performed once per week for three consecutive sessions.
Treatment Outcome
The patient experienced mild erythema, pain, and a burning sensation in the treated area during ALA-PDT.
No systemic adverse effects were reported.
Post-treatment, topical erythromycin ointment was applied for wound care.
After three ALA-PDT sessions, the lesion healed with minimal residual pigmentation, which gradually improved over time (Figure 4).
Six-month follow-up showed no recurrence, complications, or secondary malignancies (Figure 5).
Dermatoscopic re-evaluation revealed whitish irregular structureless areas with fine linear vascular structures, indicating successful lesion clearance (Figure 6).


3. Discussion
Sebaceous nevus occurs in approximately 0.3% of infants, with no gender preference, and accounts for 0.5%-1% of dermatology outpatient cases. Understanding the natural progression of sebaceous nevi is crucial for early diagnosis and treatment. The lesion typically follows a three-stage growth pattern:
Infancy to childhood: Presents as a yellow to orange, well-demarcated hairless plaque due to sebaceous gland and follicular malformations.
Adolescence: The nevus thickens and becomes verrucous due to androgen-induced proliferation of sebaceous and sweat glands. This phase is often associated with hyperkeratosis, papillomatosis, or epidermal hyperplasia.
Adulthood: The risk of secondary tumor development increases, particularly in individuals over 40 years old.
Although malignant transformation within sebaceous nevi is rare (~2.5% incidence), BCC is the most commonly associated malignancy, occurring in 0.8% of cases (8 per 1,000). Given its clinical and histological similarity to trichoblastoma, accurate differentiation is essential. Dermatoscopy aids in distinguishing between BCC and benign adnexal tumors.
Why ALA-PDT Combined with Surgery?
Due to cosmetic concerns, many patients seek dermatologic intervention for sebaceous nevi. In addition to surgical excision, alternative therapies such as curettage, electrosurgery, cryotherapy, and PDT have been explored. PDT is a non-invasive treatment widely used for skin tumors due to its excellent efficacy and cosmetic outcomes.
For tumors like BCC, surgical excision followed by multiple ALA-PDT sessions provides a dual benefit:
Complete tumor removal
Prevention of scar hypertrophy and recurrence
Since PDT has limited penetration depth, monotherapy may not completely eradicate deep tumor cells. However, combining ALA-PDT with surgical excision enhances therapeutic efficacy and significantly reduces recurrence rates.
4. Conclusion
This case report confirms that ALA-PDT combined with surgical excision is an effective and safe treatment for basal cell carcinoma (BCC) within sebaceous nevi. Future clinical studies should further explore PDT's role in managing other sebaceous nevus-associated tumors.