Psoriasis Basic Knowledge and Phototherapy
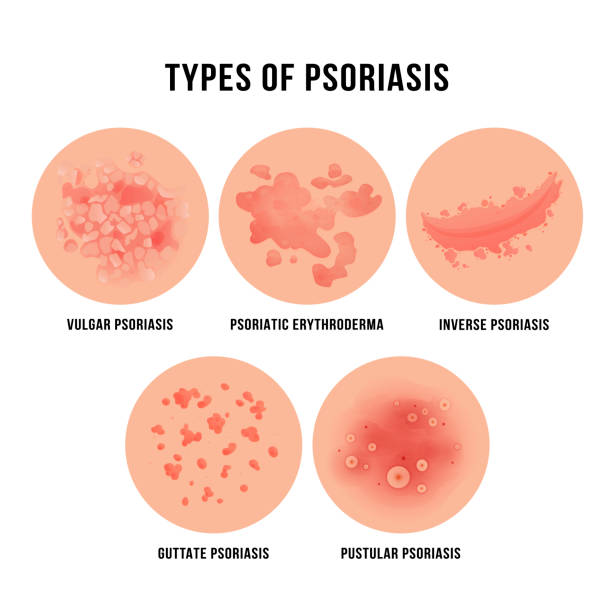
Classification of Psoriasis
Plaque Psoriasis: characterized by droplike or plaque-like lesions.
Pustular Psoriasis: either localized or generalized.
Erythrodermic Psoriasis.
Psoriatic Arthritis.
Stages of Psoriasis
Progressive Stage: existing lesions do not regress, new lesions continue to appear, prominent inflammatory changes in lesions, redness in the surrounding area, thick scales, and "Koebner phenomenon."
Stable Stage: lesions remain stable, no new lesions, milder inflammation, more scales.
Regressive Stage: lesions shrink or flatten, inflammation subsides, residual hypopigmentation or hyperpigmentation may be present.
Clinical Manifestations of Psoriasis
u At onset, it appears as small inflammatory flat papules ranging from pinhead to lentil size, gradually enlarging into coin-sized or larger, pale red infiltrated plaques with clear borders, covered with multiple layers of silvery scales.
u The morphology of lesions can vary during the disease progression. In the acute stage, lesions are often droplike, bright red, and pruritic. In the stable stage, lesions are typically plaque-like or map-like. In the regressive stage, lesions may form rings or semicircles. Some lesions exhibit thicker scales, sometimes resembling oyster shells.
u Lesions can occur symmetrically on any part of the body, with a predilection for extensor surfaces of elbows and knees and the scalp. In some cases, nails and mucous membranes may also be affected.
u Psoriasis patients with concurrent erythrodermic psoriasis are termed erythrodermic psoriasis. These cases have a small amount of exudation and are covered with moist scales. If the condition starts with small pustules and is accompanied by fever, it is called pustular psoriasis. Cases with associated joint involvement are termed psoriatic arthritis.
Phototherapy for Psoriasis
Recent research has confirmed that the therapeutic effects of phototherapy may be related to its impact on the immune system. The main immunosuppressive mechanisms involve reduced motility of antigen-presenting cells and inhibition of T lymphocyte activation. Phototherapy, especially NB-UVB, has shown outstanding efficacy and minimal side effects in the treatment of psoriasis, making it the preferred clinical choice. NB-UVB is feasible, low-risk for causing cancer, and has become a primary phototherapy method for both adults and children.
Studies have shown that 311 nm NB-UVB is more effective in clearing psoriatic lesions than broad-spectrum UVB. For the treatment of plaque psoriasis, the effective rate reaches 96.4%, with no significant adverse reactions. Regular, appropriate, and continuous NB-UVB treatment in psoriasis patients has the advantages of rapid efficacy and low side effects. Approximately 60%-75% of patients with moderate to severe psoriasis experience improvement in the extent and severity of lesions, with at least 75% improvement achieved.
FAQs about Phototherapy for Psoriasis:
Q: Which psoriasis patients should not undergo phototherapy?
A: Patients with epilepsy or lupus erythematosus should not undergo phototherapy as it may trigger these conditions. Additionally, patients with photosensitive dermatitis or photophobia should avoid phototherapy. Those taking photosensitive medications such as retinoids, antibiotics, quinolones, griseofulvin, tetracyclines, etc., should consult their doctor before undergoing phototherapy and strictly follow medical advice.
Q: What is the optimal response to treatment?
A: The optimal response after phototherapy is the appearance of mild erythema and slight pricking or burning sensation at the irradiated site 6 to 8 hours after each session, with the erythema resolving spontaneously within 48 hours.
Q: Can patients perform phototherapy at home?
A: Patients can perform phototherapy at home, but they should use phototherapy devices from reputable manufacturers. It is recommended to choose instruments with dose control for more accurate treatment. Patients should undergo a follow-up examination at the hospital after two to three months of home phototherapy.
Q: What can be done for itching after phototherapy?
A: Skin may become dry after phototherapy due to dehydration. Applying moisturizers after phototherapy helps retain skin moisture and alleviates itching.
Q: When should moisturizers be applied?
A: Moisturizers can be applied after phototherapy, and multiple applications throughout the day are allowed.
Q: Does narrowband UVB affect children's brain development?
A: No, ultraviolet rays cannot penetrate the skin to affect brain development.
Q: Is protection needed for normal skin during phototherapy?
A: Normal skin can be covered with clothing to provide appropriate protection.
Q: Are there any side effects of phototherapy, and how to deal with them?
A: Compared to medication, the side effects of UVB phototherapy are minor. The most common reaction is local skin erythema and pain, similar to sunburn, caused by excessive dosage or high-frequency irradiation. In case of sunburn, the treatment should be suspended until the erythema subsides, and then continue with therapy. For more severe erythema or blistering, patients should seek consultation with a doctor for local management before continuing the treatment.
Q: Does long-term phototherapy cause skin cancer?
A: To date, numerous studies have investigated the association between phototherapy and photodynamic therapy and skin cancer. However, no evidence has confirmed that these therapies directly cause skin cancer.
Q: What is the difference between 308nm and 311nm UV light?
A: Both 308nm and 311nm fall under narrowband UVB. The main difference lies in the intensity of the devices. 308nm UV devices have higher intensity compared to 311nm lamps, resulting in shorter treatment times, faster effectiveness, less likelihood of photoaging, and better outcomes for unconventional areas like hands and feet. In terms of treatment area, 308nm devices are typically used for precise treatment of localized, small psoriatic lesions, while 311nm devices with lamp sources can be used for larger areas, such as half-body or full-body devices, to treat extensive psoriatic lesions.
Q: What preparations should be made before phototherapy for psoriasis?
A: Patients can take a bath to reduce scale accumulation. They should prepare moisturizers in advance, as the skin may become dry after phototherapy. Avoid photosensitive foods or medications during phototherapy, as they can increase sensitivity to light and lead to excessive phototherapy or photosensitive dermatitis.
Q: Which medications can be combined with phototherapy for better results in psoriasis patients?
A: Currently, calcipotriol ointment is widely recognized as an effective topical medication. Its combination with phototherapy can shorten the time for phototherapy to take effect, reduce the number of sessions, and minimize side effects. Studies have shown that.


