When Surgery Alone Isn’t Enough: ALA-PDT Delivers a 23-Month Recurrence-Free Breakthrough for Periocular BCC
2025-04-23 15:23Case Highlights
Clinical Challenge: Periocular basal cell carcinoma (pBCC) is the most common malignancy in the periocular area, known for its aggressive and recurrent nature. Due to the unique anatomy and concerns over preserving function and aesthetics, complete surgical excision of periocular BCC is often challenging.
What’s Known: Photodynamic therapy (PDT) is effective for superficial BCC but limited by poor penetration in deep tumors. Surgical excision combined with ALA-PDT may improve outcomes.
What’s New: Palliative surgical resection combined with PDT is a feasible and effective treatment strategy for periocular BCC.
This article reports three cases of pBCC. After palliative surgical resection with either insufficient or positive margins, the patients underwent 3–5 sessions of 5-aminolevulinic acid-based photodynamic therapy (ALA-PDT), once weekly. All patients achieved clinical cure with good tolerance, no severe complications, and excellent cosmetic outcomes. During follow-up (12–23 months), no recurrence was observed.
01. Background and Objective
Periocular BCC accounts for 84%–96% of periocular tumors, involving the lower eyelid, upper eyelid, medial canthus, and lateral canthus. Though metastasis is rare, pBCC is locally invasive and prone to recurrence, potentially leading to complications such as ectropion and trichiasis. In severe cases, it can invade the orbit, resulting in extensive tissue destruction.
PDT is a noninvasive and effective therapy that selectively targets tumor cells while preserving normal tissue. Compared to traditional treatments, PDT offers excellent efficacy for superficial BCC and yields superior cosmetic results, especially for tumors in anatomically sensitive or cosmetically important areas. However, the limited penetration of topically applied photosensitizers restricts its efficacy for deep tumors.
In this study, three patients with insufficient or positive surgical margins after pBCC resection were treated with combined palliative surgery and ALA-PDT. This combination achieved favorable therapeutic and cosmetic outcomes.
02. Case Reports
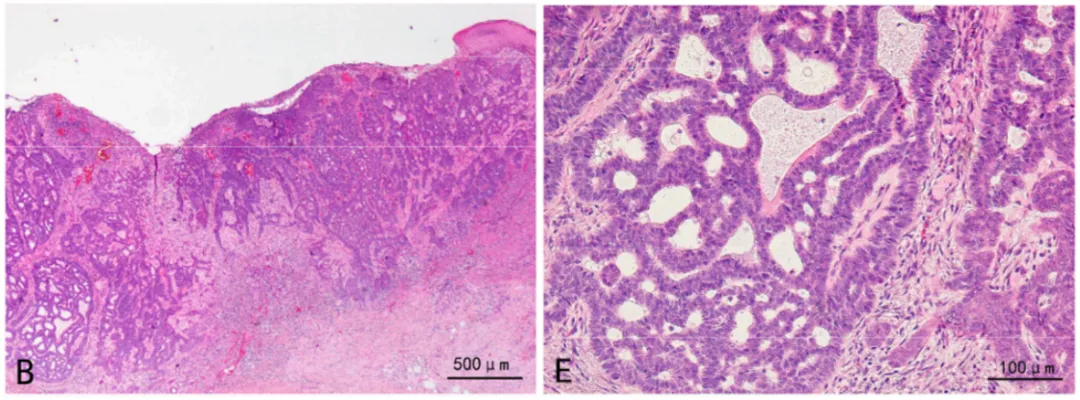
2.1 Case 1: Lower Right Eyelid BCC
Patient: 69-year-old female with hypertension and coronary heart disease.
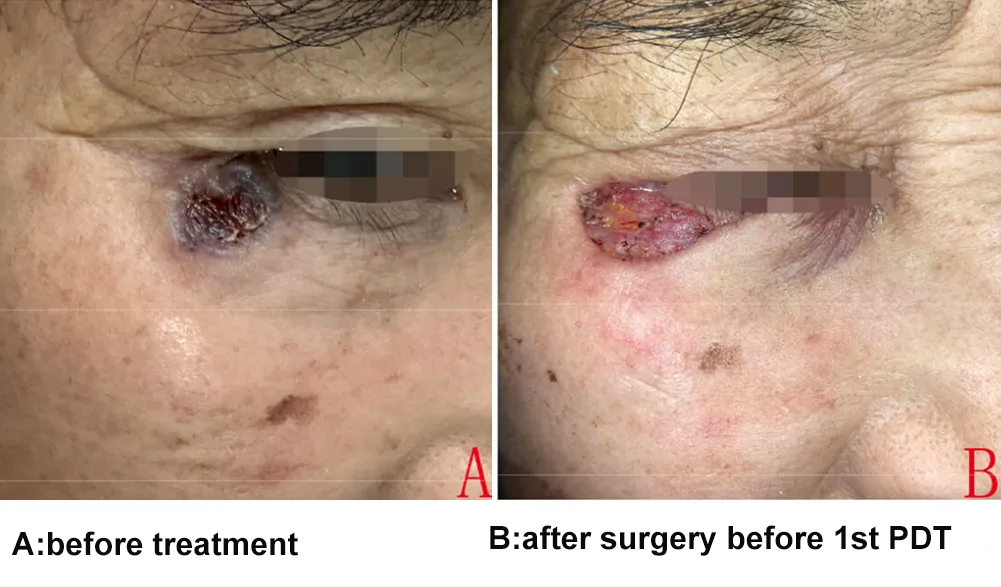
Presentation: Black lesion on the right lower eyelid, gradually enlarging over two years to ~1.2 cm, ulcerated with fluid/blood discharge.
MRI: No orbital invasion.
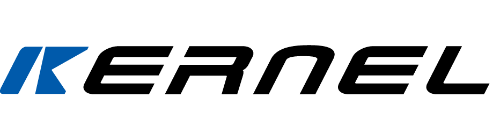
Diagnosis: BCC confirmed by histopathology.
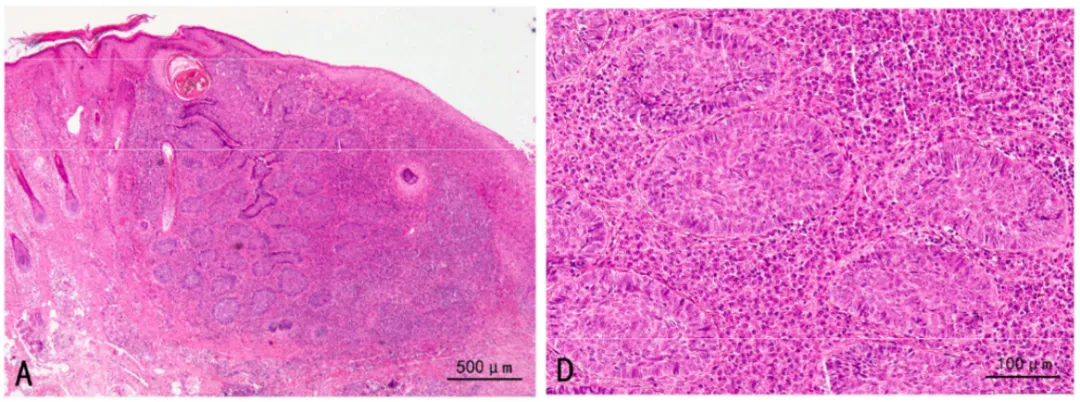
Treatment: Palliative excision + ALA-PDT. Surgical margins were close to the tumor; PDT applied directly to the open wound.
PDT Protocol: 20% ALA applied topically for 4 hours under occlusion, followed by 633nm red light at 80 J/cm² for 30 minutes. Treated once weekly for three sessions.
Outcome: No recurrence after 23 months of follow-up.
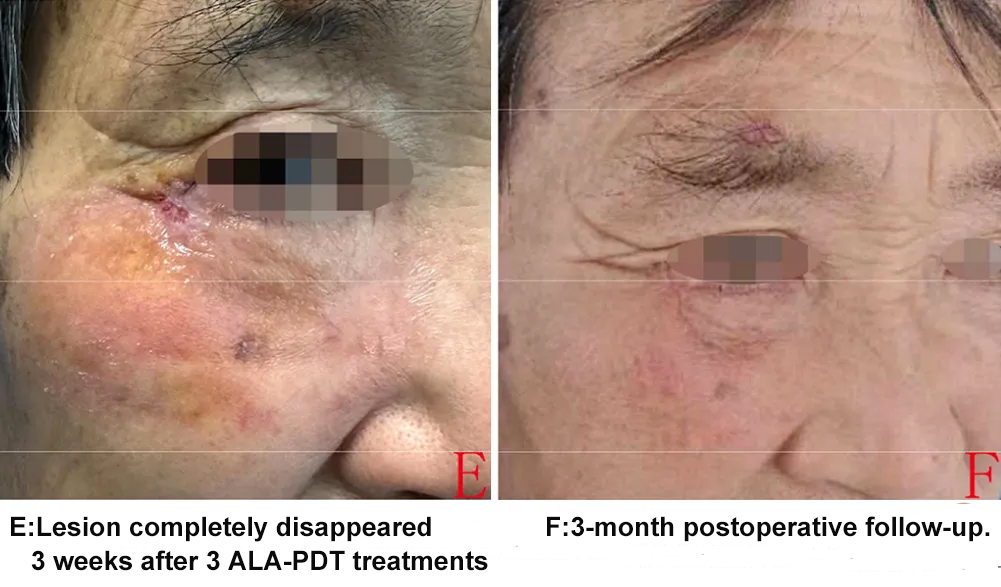
2.2 Case 2: Left Medial Canthus BCC
Patient: 70-year-old female with hysteria and psychogenic asthma.
Presentation: Deep brown nodular lesion (~1.5 cm) with scabbing and erosion; failed previous cryotherapy.
MRI: No evidence of invasion.
Diagnosis: Histopathologically confirmed BCC.
Treatment: Palliative excision + ALA-PDT. Margins appeared negative but were close to the tumor; PDT applied as a precaution.
PDT Protocol: Same as Case 1, performed weekly for three sessions.
Outcome: No recurrence after 17 months of follow-up.



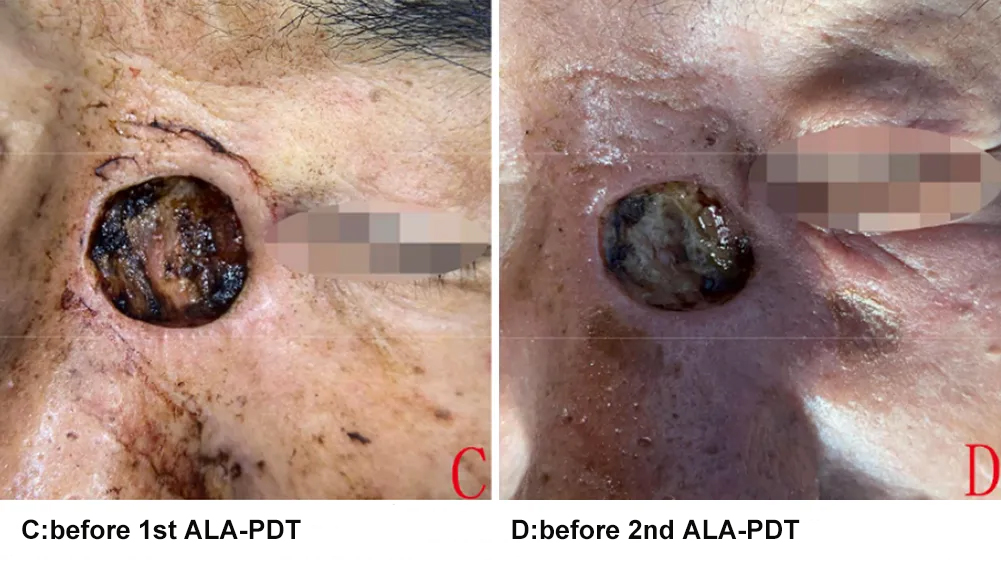
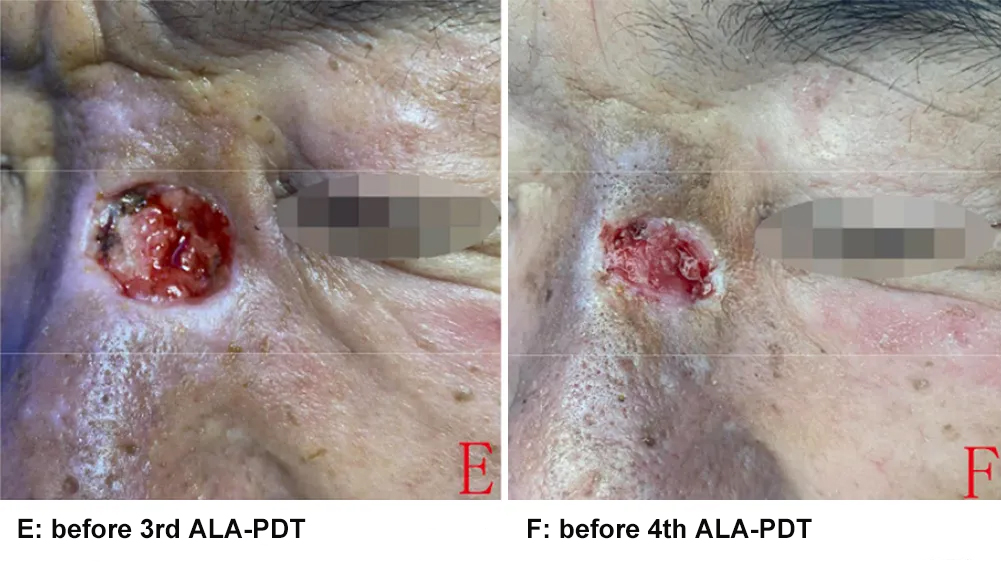
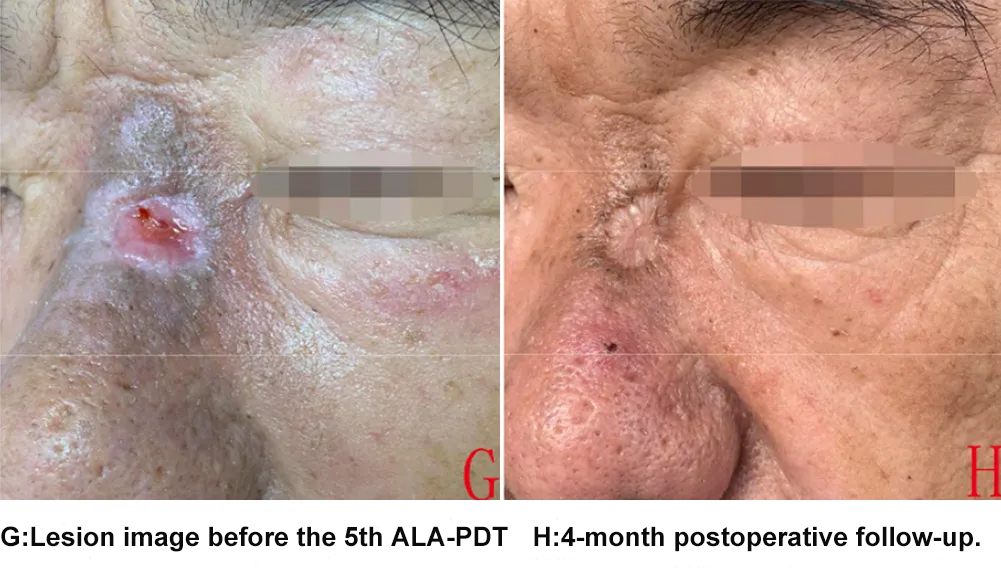
2.3 Case 3: Inferior Medial Canthus BCC
Patient: 57-year-old male with a 7-year history of untreated periocular skin lesion.
Presentation: Gray-black spot (~1.2 cm) with central ulceration.
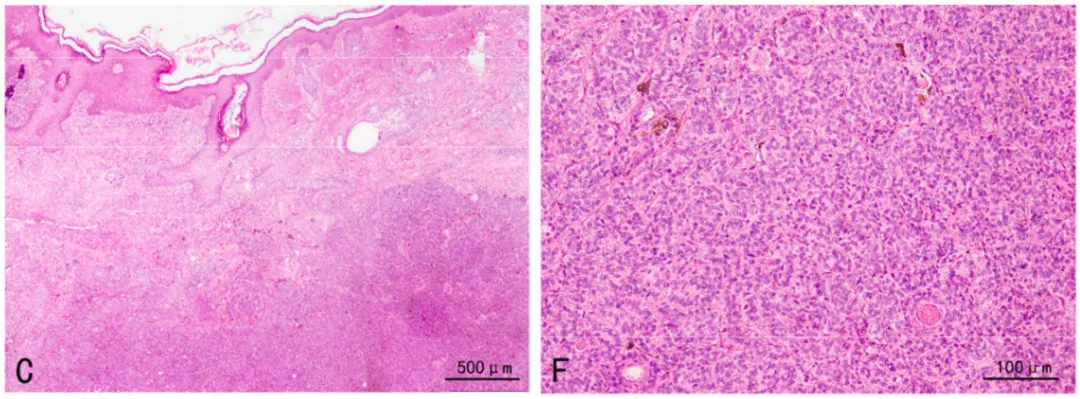
Diagnosis: BCC confirmed by biopsy; tumor showed deep infiltration and perineural invasion.
Treatment: Excision with deep positive margins followed by five weekly ALA-PDT sessions.
Outcome: No recurrence after 12 months. Minimal scarring with no functional deformity.

03. Discussion
3.1 Surgical Challenges
While surgery (especially Mohs micrographic surgery, MMS) remains the gold standard for BCC, its application in periocular areas is complex:
MMS is effective but time-consuming, technically demanding, and not always available.
Elderly patients may be unfit for lengthy procedures.
The risk of incomplete excision is higher in periocular regions, particularly the medial canthus, due to irregular tumor borders and complex anatomy.
3.2 Clinical Value of PDT
PDT is a validated, non-invasive option for treating BCC, especially superficial and low-risk nodular types. Benefits include:
High response rates
Excellent cosmetic outcomes
Tissue-sparing
Ease of administration
Repeatability
Compatibility with other treatments
Limitations: Pain during illumination, limited penetration, and higher recurrence risk in deeper tumors. These can be mitigated through combination strategies.
Preoperative PDT: Can reduce tumor size and improve surgical outcomes.
Postoperative PDT: Useful for eliminating residual disease, especially when surgical margins are inadequate and further surgery or radiotherapy is not feasible.
3.3 Combined Surgery + PDT: Efficacy and Safety
This combination is particularly valuable in pBCC cases with positive or insufficient margins:
Enhances deep tissue efficacy by improving photosensitizer/light penetration.
Allows repeated treatment with minimal trauma.
Offers superior cosmetic results with only mild scarring.
Facilitates better recurrence monitoring by avoiding flaps/grafts that could obscure evaluation.
No serious adverse events were reported aside from transient pain and pigmentation. All patients completed their PDT courses with good tolerance.
04. Conclusion
Palliative excision combined with ALA-PDT is an effective strategy for treating pBCC, offering a balance of oncologic control, cosmetic preservation, and minimized invasiveness. This combined modality holds promise, especially in anatomically challenging regions where traditional surgery alone may fall short.